-SHOULDER
Display
Herniated or Bulging Disc of the Back/Lumbar Spine
A disc is a jelly-like, fluid filled sac that acts as a cushion between the bones of your back (vertebrae). Your discs change as you age, drying out and becoming more brittle. In addition, as the discs dry out with age, the change in height between the vertebrae decreases, causing changes in posture and function. In younger adults, the center of the disc (nucleus) is held in place by many rings of the disc (picture a cross section of a tree trunk). With minor or major injuries, poor posture and strain, these rings can rupture allowing a pressing outward of the disc nucleus. Finally, as the nucleus reaches the outer edges, the disc can begin to bulge, which in turn can rub and irritate nerve roots exiting your spine.

In more severe cases, the disc can become herniated, which further presses into the spaces where nerves are exiting. Symptoms can range from localized pain, to numbness/tingling to a specific part of the back, hips, legs, or feet. In more severe cases complete lack of sensation, muscle weakness, and paralysis of an area of the lower extremity can occur. Changes in posture, strength, and range of motion can all affect the positioning of the disc and how much bulging or herniation is occurring.
How physical therapy helps
The majority of bulging and herniated discs can be treated conservatively with physical therapy. By working with your medical history, symptoms, and testing, our physical therapists can determine what areas have been affected. A thorough plan is then created to relieve pressure on the disc by improving joint function, muscle strength, and posture. Our physical therapists will often use a McKenzie based treatment program to help centralize and abolish the symptoms. Modalities, such as traction, ultrasound, or electrical stimulation may be used to reduce pain, muscle spasms, or inflammation. Our physical therapists work with you to recover lost strength and range of motion. In addition, we then train you on the correct exercises to maintain good posture and reduce the risk of future episodes.
Shoulder Pain/Shoulder Impingement
The shoulder is the most complex joint in the human body. It has to move through more than 180 degrees of motion in many directions, rotate, slide, and spin. There are a variety of muscles that have to work in concert to ensure the shoulder joint tracks properly with everyday activities. It is made up of the humerus bone, scapula (shoulder blade), and clavicle (collar bone). There are technically 4 joints that make up the entire shoulder complex.
Poor posture, weakened muscles, injury, and lack of proper range of motion can all factor into shoulder pain. Shoulder pain is typically felt in the muscles between the shoulder and neck, as well as the outside shoulder radiating down. Where your pain is can determine what structures are involved.
It is important to note that just because your pain is felt in one location, that is not usually the source of the trouble. For example, pain on the outside of the shoulder can be from an impingement of the joint or problems with the rotator cuff muscles. However, this can be caused by poor positioning and functioning of the shoulder blade, which is the real culprit. By treating the source of the problem, the irritation will resolve.
How physical therapy helps
It is important that when you have shoulder pain, you have our trained therapists evaluate your motion, strength, coordination, and joint mobility. By determining the root cause of your pain, we can then treat it effectively for fast pain relief, improved motion, strength, and return to normal activities. The goal is to restore your normal shoulder movement without pain.
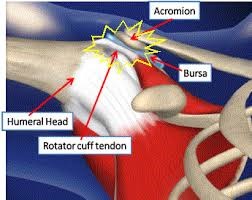
Bursitis / Tendonitis
The ending of the word “itis” is defined as inflammation. Therefore, bursitis is inflammation of a bursa and tendonitis is inflammation of a tendon. A bursa is a fluid filled sac that sits between muscles or tissues to cushion and reduce friction. In the shoulder, there is a rather large bursa between the deltoid muscle and joint. This is called the sub-deltoid bursa. This bursa can often become inflamed due to abnormal joint movements, poor posture, and weakness of the surrounding musculature. This causes strain to the tissues and excessive friction on the bursa. People tend to feel pain with movement and especially movement out to the side or reaching behind them.
Tendons connect muscles to bones. In the shoulder, common areas for tendonitis are in the rotator cuff tendons (supraspinatus, infraspinatus, teres minor, and subscapularis) and bicep tendons. Pain can be felt deep in the shoulder or in the front of the shoulder. Pain is usually felt as a sharp, catching sensation with certain movements.
How physical therapy helps
Physical therapy is the first line of conservative treatment for bursitis and tendonitis. Since most bursitis and tendonitis issues are due to underlying abnormal mechanics of movement and weakness, our trained physical therapists evaluate your movement to pinpoint the exact source of the trouble. Modalities may be used to alleviate pain and discomfort, while hands-on therapy improves joint mechanics and movement. Finally, strengthening exercises and joint coordination exercises help to restore stability to the affected area and to prevent re-occurrence of the symptoms.
Sports Injuries
Whether you are a professional athlete, high school athlete, or just like to be active and play sports, injuries can occur. Many shoulder sports injuries occur because of a fall onto an outstretched arm or from repetitive overhead actions, such as swimming, tennis, softball, or baseball. Another reason for shoulder sports injuries is an imbalance which can occur in certain groups of the shoulder muscles if one group of muscles is stronger than another. For example, an athlete that has strong chest muscles, but weak rotator cuff muscles, can put themselves at risk of injury.
How physical therapy helps
Our physical therapists are experts at caring for and rehabilitating sports injuries. Our goal is to rehabilitate you back to your favorite sports activities pain-free as quickly and safely as possible. Sports injuries require unique care and rehabilitation, therefore, know that you are in the right hands with us. From mild sprains to recovery after surgery, we have you covered.
Rotator Cuff Injuries
The rotator cuff is a group of muscles surrounding the shoulder. They are made up of the supraspinatus, infraspinatus, sub-scapularis, and teres minor muscles. While these muscles are small and not that powerful, they play a critical role in how the shoulder moves. Without your rotator cuff, you would not be able to lift your arm very far from your side. The job of the rotator cuff is to guide the direction of the humerus head down and spin so that it clears the bony shelf above the socket called the acromion. When the rotator cuff is weak, the head of the humerus rides up slamming into the acromion above it.
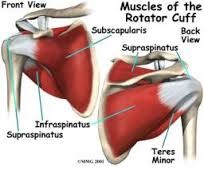
The rotator cuff takes a lot of abuse over a lifetime and tearing is very common as we age. Many factors can lead to injury to the rotator cuff such as sports injuries, falls onto the shoulder or arm, repeat lifting or movements, poor posture, or heavy lifting in abnormal positions.
Rotator cuff tears can be minor, causing pain and inflammation, or major which can require surgery. With surgery, depending on a variety factors such as the quality of the tissue, the extent of the tear, and other health factors, the recovery can take between 3-6 months. Physical therapy is a very important part of preparing for surgery and rehabilitating after surgery.
How physical therapy helps
Often, with small tears, physical therapy can dramatically reduce pain, improve function, and allow you to lead an active lifestyle without any problems. Our physical therapists will work with you to improve your shoulder range of motion, restore proper joint mobility, reduce inflammation, relieve pain, and improve the strength of your rotator cuff.
If surgery is needed, we work closely with your physician to follow his/her protocol on rehabilitation. The beginning of therapy focuses on reducing pain, education on protection of the surgery repair, and maintaining a certain range of motion. Over time, as your physician protocol allows, range of motion is increased, joint mobility is restored, and finally strengthening is begun.
Towards the end of your physical therapy, further strengthening and complete range of motion will be attained for your shoulder. All of this is coordinated per the instructions of your physician and we ensure thorough communication with your physician at all times.
Frozen Shoulder / Adhesive Capsulitis
Frozen shoulder is a painful shoulder joint condition. In medical terminology it is called “adhesive capsulitis”. How frozen shoulder exactly begins is still a bit of a mystery, however, it typically occurs after a trauma or repetitive injury to the shoulder. Women in the pre and post-menopausal age range are more likely to experience frozen shoulder, however, men can also experience frozen shoulder.
With frozen shoulder, the thick capsule of tissue that surrounds the shoulder joint begins to experience chronic inflammation. The body begins a cycle of inflammation and scarring that causes the capsule around the shoulder joint to contract and become limited in its flexibility. This causes very painful range of motion in the shoulder when trying to move the arm.
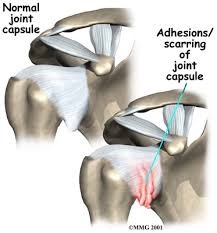
At the beginning of frozen shoulder, it is very painful and range of motion becomes limited. This can be around 4–8 weeks in duration. After that, motion is very limited in the shoulder, but often not as painful. Depending on the severity of the condition, it can take sometimes up to a year to resolve and improve range of motion.
How physical therapy helps
Physical therapy can make a big difference in shortening the time it takes to recover from frozen shoulder (adhesive capsulitis). By coming to therapy as early as possible, the inflammatory cycle can be significantly reduced, limiting scarring and contraction of the shoulder capsule. In turn, physical therapy, along with medication, can limit the pain and ensure a faster recovery.
Our physical therapists work with many frozen shoulder patients to reduce pain quickly and restore range of motion to the shoulder. Physical therapy treatments focus on hands-on therapy and specialized exercises to maintain as much range of motion as possible during the inflammatory phase of frozen shoulder. During the “thawing” phase, we work with you to improve range of motion in your shoulder and restore strength. It can take quite awhile for the motion to be restored to the shoulder, but by coming to physical therapy, we can help you recover as quickly as possible.
Labrum Tear
The labrum is a thick ring of cartilage around the socket part of your shoulder joint (glenohumeral joint). The labrum acts like a cup for the head of the humerus to sit in (like a ball inside a cup). The labrum gives stability to the joint and also helps to cushion as the shoulder joint moves.
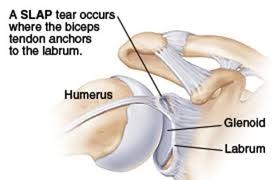
The labrum can tear with injury from a blow to an outstretched arm or from repetitive injuries overhead. Sometimes, a labrum tear can be involved when the rotator cuff is torn. A common tear is called a SLAP lesion (Superior Labral tear from Anterior to Posterior). This is a tear of the labrum from the top part in front to back. This often needs surgical repair, and we work with your physician on their protocol to rehab your shoulder after surgery.
How physical therapy helps
Most often, labral tears are fixed surgically and need physical therapy after the procedure. We work very closely with your physician to follow their protocols for rehabilitation to your shoulder. Physical therapy involves a progression of your range of motion per the protocol, and towards the end, restoring of your motion. In the meantime, pain, swelling, and function are addressed.
display
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Dislocation, Instability
Dislocation of the shoulder typically occurs from falling onto an outstretched arm or a blow to the side or back of the shoulder when falling on it. This can happen in different sports activities or falls. Dislocations are managed medically to relocate the head of the humerus bone. Depending on the severity of the dislocation, your physician will typically prescribe physical therapy to help stabilize the shoulder joint and protect it during a recovery phase.
With frequent dislocations, the shoulder can become unstable as many structures in the shoulder get damaged and become too lax. By strengthening the muscles around the shoulder, stability can be increased in the shoulder, preventing future dislocations.
At times, dislocations can be quite severe and lead to tearing of cartilage, tendons, ligaments, or muscles. In this case, surgery is often needed. After surgery physical therapy is an important part of recovery and returning to normal activities.
How physical therapy helps
Physical therapy is very important after a dislocation. Our physical therapists work with you closely to protect the joint while it heals, teach you how to take care of your injury, and gently rehabilitate your shoulder. During the healing phase, your shoulder will be protected and pain will be addressed.
Per your physician’s protocol, we will gradual increase your range of motion, maintaining your joint stability. Further into therapy, gentle strengthening is performed to improve the muscle support around the shoulder. Ideally, full range of motion and strength is recovered, allowing you to return to normal activities and with the knowledge to protect your shoulder from further injury.
Sprain / Strain
Shoulder Sprain / Strain
A sprain in the shoulder involves the ligaments, and a strain involves the muscles around the shoulder. A sprain / strain typically occurs because the tissue has been overstretched too quickly, resulting in micro-tearing of the tissue. This results in painful inflammation, typically increased with movement and use of the damaged tissue.
The damage from a sprain / strain can be minor or major, depending on the severity of the injury, person’s health, and age. As we age, our tissue becomes less elastic and becomes more prone to tearing.
How physical therapy helps
Physical therapy is a very important part of the recovery from a sprain / strain. First, the focus is on reducing pain and inflammation while maintaining or regaining range of motion. After the inflammatory phase is coming to an end, the focus shifts to attaining full range of motion then gradual strengthening of the injured areas to regain normal strength. Towards the end of treatment, focus is shifted to the coordination of the shoulder joint and education towards preventing future injury. If you have suffered a sprain or strain, call us today as soon as possible to start feeling relief and getting back to normal activities.
Fractures
Shoulder Fractures
Fractures in the shoulder occur for a variety of reasons, but typically from a fall onto the shoulder itself. Fractures can occur in seniors also due to osteoporosis (thinning and weakening of bone).
 The goal with fracture management is to provide a safe position for the bone to heal (typically around 8 weeks), while maintaining range of motion. As the bone heals, strengthening can begin and rehabilitation back to normal activities is progressed.
The goal with fracture management is to provide a safe position for the bone to heal (typically around 8 weeks), while maintaining range of motion. As the bone heals, strengthening can begin and rehabilitation back to normal activities is progressed.
At times, surgery may be needed to hold the bone together with plates or screws. This stabilizes the bone, but does disrupt muscles and leads to more weakness in the shoulder muscles. Physical therapy is very much needed after this to restore normal range of motion and strength to the shoulder. Recovery times can vary, but traditionally take 12–16 weeks.
How physical therapy helps
Physical therapy is a very important part of rehabilitation after a shoulder fracture. Whether you are a young person or older, we work closely with you and your physician to make sure your fracture is protected while it heals. We then work closely with you to gradually restore your range of motion, relieve pain, soothe aching muscles, and improve your strength. The goal of physical therapy is to return you to normal activities after the normal course of bone healing. We can prevent long-term damage and address any issues that may have caused a fall onto the arm in the first place.
Post-surgery Rehab
Shoulder Post-surgery Rehab
There are a variety of shoulder surgeries that may have to be done in order to stabilize the shoulder or repair damaged tendons or ligaments. With the advances in arthroscopic surgery, recovery times for shoulder injuries have improved, however, physical therapy is still needed to reduce pain quickly, restore range of motion, improve strength, and return the individual to the normal activities they like to do.
How physical therapy helps
Post-surgery recovery can be difficult on sleeping, bathing, dressing, and many other normal daily activities we take for granted. Our physical therapists work with you to teach you how to adapt to these activities of daily living while recovering.
Physical therapy focuses on providing you with inflammation and pain control to reduce your pain as quickly as possible while you are recovering. The surgical process can often leave muscles cramped and irritated. Our gentle hands-on therapy is perfect for soothing sore muscles and restoring normal muscle movement.
We work closely with your physician on the correct protocol to rehabilitate your shoulder after surgery. Every person’s surgery is unique, and rest assured, your recovery is treated as such. According to your protocol, we will help restore your range of motion, increase your strength, and help you return to normal activities using your shoulder.
Total Shoulder Arthroplasty
A total shoulder replacement is becoming a much more common procedure over the past several years. In shoulder replacement surgery, the damaged parts of the shoulder are removed and replaced with artificial components, called a prosthesis. The treatment options are either replacement of just the head of the humerus bone (ball), or replacement of both the ball and the socket (glenoid). The exact type of replacement will be determined by you and your physician for what is best for you.

A careful, well-planned rehabilitation program is critical to the success of a shoulder replacement. You usually start physical therapy soon after the operation. Your surgeon or physical therapist will provide you with a home exercise program to strengthen your shoulder and improve flexibility. Protocols set forth by the physician are followed closely by our physical therapists for a successful outcome.
