-HIP
Display
Herniated or Bulging Disc of the Back/Lumbar Spine
A disc is a jelly-like, fluid filled sac that acts as a cushion between the bones of your back (vertebrae). Your discs change as you age, drying out and becoming more brittle. In addition, as the discs dry out with age, the change in height between the vertebrae decreases, causing changes in posture and function. In younger adults, the center of the disc (nucleus) is held in place by many rings of the disc (picture a cross section of a tree trunk). With minor or major injuries, poor posture and strain, these rings can rupture allowing a pressing outward of the disc nucleus. Finally, as the nucleus reaches the outer edges, the disc can begin to bulge, which in turn can rub and irritate nerve roots exiting your spine.

In more severe cases, the disc can become herniated, which further presses into the spaces where nerves are exiting. Symptoms can range from localized pain, to numbness/tingling to a specific part of the back, hips, legs, or feet. In more severe cases complete lack of sensation, muscle weakness, and paralysis of an area of the lower extremity can occur. Changes in posture, strength, and range of motion can all affect the positioning of the disc and how much bulging or herniation is occurring.
How physical therapy helps
The majority of bulging and herniated discs can be treated conservatively with physical therapy. By working with your medical history, symptoms, and testing, our physical therapists can determine what areas have been affected. A thorough plan is then created to relieve pressure on the disc by improving joint function, muscle strength, and posture. Our physical therapists will often use a McKenzie based treatment program to help centralize and abolish the symptoms. Modalities, such as traction, ultrasound, or electrical stimulation may be used to reduce pain, muscle spasms, or inflammation. Our physical therapists work with you to recover lost strength and range of motion. In addition, we then train you on the correct exercises to maintain good posture and reduce the risk of future episodes.
Hip Pain and Thigh Pain
Hip pain is typically felt in 3 places, the groin, outer hip or deep buttock. Depending on where the pain is, focus corresponds to the dysfunction around that area. The hip joint is incredible as it moves through a large range of motion, while bearing the weight of the body and providing stability.
Most hip pain stems from limited motion of the hip causing abnormal pressures to different muscles, tendons, or ligaments around the area. With acute pain, it can be felt deep in the groin or outer hip. However, with more severe irritation, radiating pain can even be felt into the thigh or knee.
Having flexible hip joints with strong muscular support is key to a healthy back. When the hips don’t move like they should, the normal forces of walking, bending, and squatting are transferred to the spine instead of the hips.
How physical therapy helps
Physical therapy can quickly relieve hip and thigh pain. Our physical therapists perform a thorough evaluation to determine exactly where your pain is coming from. By assessing your hip range of motion, strength and joint mobility, we determine where your limitations are and formulate a treatment plan that will take care of the root cause.
By improving your joint mobility, strength and range of motion, we help you restore normal pain-free walking and activities.
Sciatica
Sciatica is a term used to describe radiating pain into the buttock that may travel down the back of the thigh. Often this pain is achy and spread out along the buttock and back of the thigh.
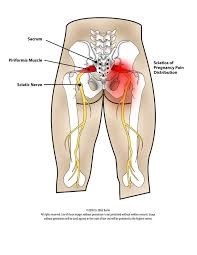
Sciatica typically comes from irritation to the sciatic nerve, which travels deep in the buttock and down the back of the leg. In about 20% of people, the sciatic nerve pierces through the piriformis muscle deep in the buttock, instead of underneath it. This muscle helps guide hip movement, but can become very tight with prolonged sitting, which causes pressure and irritation to the sciatic nerve resulting in pain.
Radiating pain to the leg doesn’t necessarily mean you have sciatica, but it does tell you that something is wrong. Irritated muscles and tissue often can radiate pain. Spread-out, achy pain is often indicative of this type of problem. Sharp, stabbing pain with numbness or tingling is more nerve irritation or compression occurring in the back or leg. This typically occurs more to specific parts of the leg.
How physical therapy helps
Physical therapy is one of the best treatments for sciatica and radiating pain into the leg. It first takes a thorough evaluation to determine where your problem is stemming from. Our physical therapists take time to examine the movement of your spine, hips, and legs. Range of motion, strength, joint mobility, and muscle condition are assessed by our medically trained physical therapists.
After we determine the root cause of your problem, we generate a comprehensive treatment plan to quickly relieve your pain, radiating symptoms, improve range of motion, improve strength, and help you to prevent future episodes.
With specialized hands-on techniques, we improve your spinal and hip mobility, which reduces pressure on your sciatic nerve. In addition, modalities such as heat, ice, electrical stimulation, and ultrasound may be used to reduce inflammation and resolve your pain quickly. We also perform stretching and strengthening exercises to restore your normal motion and strength, resulting in lasting effects that will stop your pain from returning.
Osteoarthritis of the Hip
Osteoarthritis of the hip can be painful as the hip is needed to move with sit to stand, walking, squatting, and bending. The hips take a lot of wear and tear over the years leading to a degeneration of the cartilage that lines the joint. As the cartilage wears over time, the joint becomes stiffer and the muscles of the buttocks generally weaken over time. This compounds the effects on the hip causing grinding and wearing. In advanced stages, bony spurs can form around the joint and even change the shape of the joint.
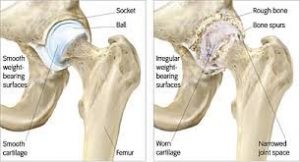
Most minor to moderate cases of hip osteoarthritis can highly benefit from physical therapy. In advanced stages, a total or partial hip replacement may be needed to repair the damaged joint. Physical therapy in the hospital and outpatient facilities is highly important in the recovery from a hip replacement surgery.
How physical therapy helps
The pain associated with osteoarthritis of the hip comes from inflammation in and around the joint from wear and tear. Tight muscles, tendons, ligaments, and tissues occur with osteoarthritis further limiting joint movement. In addition, weakness of the buttock muscles and hip rotators generally occurs because of the loss of movement.
Physical therapy can improve joint mobility, range of motion, and muscle strength. Our hands-on therapy and specialized exercises normally achieve a marked improvement in your hip range of motion. First, we thoroughly evaluate the mechanics of your hip joint, walking, and hip muscle coordination. By pinpointing the specific areas that need attention, we formulate a plan to quickly relieve your pain, improve your motion and walking.
Trochanteric Bursitis
The ending of the word “itis” is defined as inflammation. Therefore, bursitis is inflammation of a bursa and tendonitis is inflammation of a tendon. A bursa is a fluid filled sac that sits between muscles or tissues to cushion and reduce friction. In the hip there is a rather large bursa on the outside between the bony area (tronchanter) and the thick band of tissue stretching from your hip to your knee (iliotibial band). This is called the tronchanteric bursa.

This bursa can often become inflamed due to abnormal joint movements, poor posture, and weakness of the surrounding musculature. This causes strain to the tissues and excessive friction on the bursa. People tend to feel pain with prolonged walking or standing. It is often, very tender to touch on the outer hip and thigh.
How physical therapy helps
Physical therapy is the first line in conservative treatment for trochanteric bursitis. Since most bursitis is due to underlying abnormal movement and weakness, our trained physical therapists evaluate your movement to pinpoint the source of the trouble. Modalities may be used to alleviate pain and discomfort, while hands-on therapy improves joint mechanics and range of motion.
Finally, gentle strengthening exercises and joint coordination exercises help to restore stability to the affected area and prevent re-occurrence of the symptoms.
Total Hip Replacement / Partial Hip Replacement
When the hip has suffered a significant trauma such as a fracture or with long-term arthritis that is affecting your ability to move and walk, a total hip replacement surgery may be needed. In a total hip replacement surgery, the socket of the hip joint and head of the femur are replaced. With a partial hip replacement either the head of the femur is replaced or the socket of the hip. There have been many advances in the technology of the total hip replacement prosthesis and procedures allowing for less invasive surgery and faster recovery times.
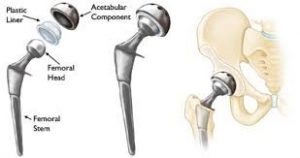
Typically, people have suffered for awhile before having surgery, leading to changes in walking, muscle strength, and function. Physical therapy before surgery in general has shown to help the speed and quality of recovery after surgery.
How physical therapy helps
Working with your physician’s protocols, we coordinate a thorough rehabilitation program to get you back to normal walking as soon as possible.
Typically, you may start physical therapy in the hospital the day after your procedure. In the hospital, basic movements and function such as getting up and down out of chairs, basic walking, and strength are addressed. After discharge from the hospital, the doctor may recommend further therapy in the out-patient clinic. Here, we complete the rehabilitation cycle, further restoring your range of motion via your physician’s protocols, restoring normal walking, balance, hip coordination, and alleviating pain. We continue to reinforce safety precautions with your hip movement while you heal. The end result of physical therapy is being able to return to most normal activities pain-free.
Sprain / Strain
Sprains refer to injuries of the ligaments (connect bone to bone) and strains refer to injuries of the muscles or tendons (connect muscle to bone). Sprains and strains occur from quick over-stretching of the tissues causing micro-tearing and subsequent injury. Swelling begins as part of the inflammation process, causing pain, and difficulty with movement.
The first step in treating sprains or strains in the hip is to rest and ice. With severe limitations in movement, you should see your physical therapist right away. There are different levels of sprain or strain from mild to severe. In some cases, the tearing can be complete and even be in need of surgical repair.
How physical therapy helps
In most cases, physical therapy can effectively help you recover from a sprain or strain. We first evaluate the injured area to determine the extent of the injury and ensure that the ligaments or tendons are still intact. After we pinpoint the injured area, we formulate a treatment plan that will quickly relieve your swelling, pain, and begin restoring range of motion.
The goal of physical therapy is to restore your normal range of motion and restore normal strength. If you participate in sports or are very active, we work closely with you to make sure you fully recover and can participate in those activities you love to do.
display
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Post-surgery Rehab
Other types of surgeries for the hip are fracture repairs using pinning or repair from trauma. The amount of force it takes to break bone means that the soft tissues around the hip are most likely significantly injured also. After surgery, due to limited movement, range of motion is lost as well as strength, rather quickly. Since walking is a very complex action of different muscles moving in a coordinated action, it can be difficult to walk after a hip surgery.
How physical therapy helps
Physical therapy is an important part of the rehabilitative process after a hip surgery. Depending on your surgery and your physician’s protocols, we will gently progress you through a structured rehabilitation program. The goal is to restore pain-free range of motion in the hip while maintaining surgery recovery protocols. Finally, walking coordination, balance, and strength are improved so you can return to normal pain-free walking.
Difficulty Walking
It takes us at least 12 months as a baby to learn the fundamentals of walking. It takes even longer to learn how to walk properly and eventually run. Walking is very complex and requires good balance, the ability to know where your joints are in space (proprioception), the ability to know how your joints are moving (kinesthesia), good range of motion, and strength.
As we age, with declining activity, or after an injury, walking can become difficult. With previous injuries or pain in the knee or hip, our walking pattern can change leaving us with a limp or even worse, back pain. Changes in posture can also be responsible for changes in walking patterns.
When walking patterns change, abnormal stresses and strains with everyday activities can be transmitted to areas it shouldn’t. For example, if you have knee pain and you begin to limp, the other hip and your spine now have to take double the weight. This can lead to pain and dysfunction in those areas also. The good news is that if you have difficulty walking, you can be helped. Physical therapists are the experts uniquely trained to do so.
How physical therapy helps
One of the main specialties of physical therapy is helping people to walk normally. We complete a thorough evaluation of your range of motion, strength, walking patterns, balance, and coordination. By discovering what area you have difficulties, we can paint a picture of why your walking is not as it should be.
We then coordinate a treatment plan that will address your range of motion, pain, coordination, balance, and strength. The end result is the ability to walk without the need of an assistive device such as a cane or walker, safely and smoothly.
Incontinence
Urinary incontinence is the leakage of urine at inappropriate times. With incontinence, you may have trouble starting the urine stream or holding urine when you feel a strong urge to go.
Urinary incontinence involves the muscles of the pelvic floor. These muscles attach to the bottom of the pelvic bones and run front to back, forming a bowl-like structure that lifts to support the internal organs and controls the sphincter muscles. The pelvic-floor muscles also help support the low back, stabilize the pelvic bones, and help with sexual function. Women are more likely than men to have urinary incontinence, but men can have it too.
How physical therapy helps
There are different types of incontinence, so after the therapist’s evaluation, they will develop an individual treatment program just for you. Using pelvic-floor exercises, your therapist will help you strength those muscles so that you can better control your bladder. They will also show you how to “find” the right muscles and use them correctly.

Your physical therapist can also provide information about diet and nutrition to avoid food and drinks that may irritate the bladder. They will also provide information about changing behaviors that make symptoms worse. Lastly, they can help you find ways to decrease urinary urge and frequency.
Piriformis Syndrome
The piriformis muscle is deep in the buttocks and helps with rotating the hip. The sciatic nerve typically dives underneath the piriformis muscle as it makes it way down to the leg. With excessive sitting, loss of movement in the hips or trauma, the piriformis muscle can press down onto the sciatic nerve. Typically, mild symptoms cause aching deep into the buttock and often radiating pain to the outer thigh. With more severe cases, tingling, numbness, or severe pain can radiate down the thigh.
How physical therapy helps
Physical therapy is very effective in treating piriformis syndrome. By analyzing your hip range of motion, muscle function, walking, and posture we can determine the right approach to treating the affected area. With specialized hands-on therapy and specific exercises we help regain lost range of motion, reduce pain quickly, and improve symptoms into the leg. We teach you easy to do exercises and modified activities you can do at home to prevent the re-occurrence of the symptoms.
